Contributor score: 1206
don't just do something, stand there!
This is a corrected version of the post from @abhishek021196 below (https://nbmeanswers.com/exam/free120/1426#3919).
Fragile X syndrome X-linked dominant inheritance. Trinucleotide repeat in FMR1 gene = hypermethylation = decreased expression.
Most common inherited cause of intellectual disability (Down syndrome is the most common genetic cause, but most cases occur sporadically).
Findings: post-pubertal macroorchidism (enlarged testes), long face with a large jaw, large everted ears, autism, mitral valve prolapse, hypermobile joints.
Trinucleotide repeat expansion [(CGG) n ] occurs during oogenesis.
Responding to @azibird’s comment:
Another way to read the stem is like this: “Assume you will make a statement that assures mom that boy is fine. What other statement do you want to make?”
Since we’re *already* assuring mom, the best next thing is to ask an open-ended question. There’s a reason for this. As a physician, you really don’t want to say more than what you are (1) sure of or (2) obliged to.
“Accept him as he is” = judgy.
“He’s not going to get any taller” = you don’t know this for sure.
- A: Broca’s
- B: Premotor
- C: Motor
- D: Somatosensory
Damage to C (motor) wouldn’t explain fluency problems. Fluency (=Latin flow; the ease with which the brain formulates words). Slurred speech is your brain knowing and formulating the words easy but your mouth muscles not co-operating!
So, dis-fluency ≠ slurred speech. This gentleman is dis-fluent in the same way you’re dis-fluent when you visit Paris: your brain struggles to formulate French words in the first place! The only lesion that explains that in your native tongue is a lesion to the language synthesis center = Broca’s area.
“It’s awfully quiet in these here pages ...” 🌵🤠
---
“It’s awfully quiet in these here pages ...” 🌵🤠
---
The CFTR protein is a transmembrane protein. Like all proteins, its translation begins in the cytosol; that said, CFTR contains an N-terminus “signal sequence”, which means as it is being translated, it (and the ribosome making it!) will be transported to the Endoplasmic Reticulum.^footnote!
As it gets translated, its hydrophobic motifs will emerge, which embeds the CFTR protein within the phospholipid bilayer of the ER itself! That means the protein will never again be found “in the cytosol” because it gets threaded through the bilayer (which is, in fact, how all transmembrane proteins become transmembrane proteins at the cell surface -- they have to be made into transmembrane proteins in the ER first!).
So, yes, ultimately, these misfolded proteins will be directed toward a proteasome for degradation/recycling, but that will happen as a little vesicle (or “liposome”); the misfolded protein, in this case, is not water-soluble (since, by definition, it has hydrophobic motifs which get “threaded through” a bilayer to create the transmembrane pattern), which means you won’t find it in the cytosol.
\ footnote! \ The hitching of active* ribosomes to the Endoplasmic Reticulum is why we call that area of ER “rough Endoplasmic Reticulum (rER)”; on electron microscopy, that section was bespeckled with little dots; later, we (humans) discovered that these dots were ribosomes!
\ * \ By “active ribosomes”, I just mean ribosomes in the process of converting mRNA to protein! (What we call “translation” ;)
For a great little summary of the Endoplasmic Reticulum (and many other concepts in molecular biology!), see this from Alberts’ Molecular Biology of the Cell:
https://www.ncbi.nlm.nih.gov/books/NBK26841/#A2204
The prevailing rule of American medicine (and law) is individual autonomy, otherwise known as liberty. In American law, no other person, professional or otherwise, is granted “default access” or privilege to another person’s body—that includes the physician! (It even includes spouses! That’s why, in American law, you can be married to someone and still be charged with sexual assault/rape; marriage ≠ your spouse surrendering “bodily rights”.) The physician must receive consent from “a (conscious) person” before they become “a (conscious) patient”. In the same way, the person (now, patient) must give consent before anyone else is permitted to be involved in his or her care—spouses included!
Accuracy means the data points are dispersed, but when you take the mean of those points, that mean (“sample mean”) is nearby the population mean (“true mean”). Data points are “more precise” if the dispersion across data points is smaller than some other set of data points (notice how this is a comparison and not an “absolute” statement); precision says nothing about how close the average of the data points are to the “true mean.”
Keep in mind that accuracy and precision are relative descriptors; you can’t say “so-and-so is precise”; no, you can only say “such-and-such is more precise than so-and-so” or “so-and-so is more accurate than such-and-such.” So, in this case, we can infer that NBME considers “men at the urologist” to have BUNs that are closer to each other (more clustered; more precise; less dispersed) than the BUNs of “men at mall.”
Here’s a nice image:
https://medbullets.com/images/precision-vs-accuracy.jpg
The reason something is an “autosomal recessive” disease is because the protein encoded by the gene (of which you have two alleles, of course) does something where as long as you make SOME protein, your body should be okay.
That’s kind of vague, so take the case of Cystic Fibrosis: you don’t present with Cystic Fibrosis if you have at least one functional allele -- that’s because CFTR protein is a protein that (in the case of bronchiole tissue) moves Cl- from inside cells to the outside lumen, which brings with it H2O and keeps the bronchiole lumen nice and watery, and fluid and non-viscous and non-pluggy.
So long as you make enough of this protein, you don’t “need” both alleles to be good; the good allele can “make up for” (make enough of the protein product to compensate for) the “broken allele.” So, once again, understanding the pathophys of a disease allows you to reason through and predict things like disease penetrance and expressivity.
You have to think about it this way: the basement membrane is the “scaffolding” on which [restorative] healing occurs. So, yes, stem cells (type II pneumocytes) would be involved in that healing process but they couldn’t restore the normal architecture (“no abnormalities”) without the ‘skeleton’ of the basement membrane telling them where to go, in what direction to grow, which way is “up”, etc. If the basement membrane is destroyed, you can still get healing, but it won’t be organized healing -- it’ll be disorganized healing, which does not appear as normal tissue. (Disorganized healing is better than no healing, but without a BM, the regenerating cells don’t have any “direction” and therefore can’t restore the normal architecture.)
If I gave you a bucket of spontaneous pneumo patients -- and you reached your hand in there and pulled one out -- what scenario would be more common: In your hand you have a smoker or in your hand you have a thin male? It’s the latter.
You have to think about this using the concept of CONDITIONAL PROBABILITY. Another way to ask this type of question is like this: “I show you a patient with spontaneous pneumothorax. Which other thing is most likely to be true about that person?” Or you can phrase it these ways:
- Given a CONDITION (
spontaneous pneumo), what other finding is most likely to be the case? - Given a pool of people with spontaneous pneumothorax, what other thing is most likely to be true about them?
In other words, of all people who end up with spontaneous pneumo, the most common other thing about them is that they are MALE & THIN.
If I gave you a bucket of spontaneous pneumo patients -- and you reached your hand in there and pulled one out -- what scenario would be more common: In your hand you have a smoker or in your hand you have a thin male? It’s the latter.
Calculations for dad. The probability of the father being a carrier is 2/3 since it is known that he doesn’t have the disease. Then the probability of him passing it on to his kid is 1/2, thus:
- Probability of dad being carrier = 2/3
- Probability of dad passing on disease allele = 1/2
Calculations for mom. With the Hardy-Weinberg Principle, you can figure out the probability of the mother being a carrier:
q = sqrt(1/40,000) = 1/200
So, 2pq = 2 * 1/200 * 199/200, which is approx 1/100.
For the child to get the allele from mom, two things need to happen: (1) mom must be a carrier [“heterozygote”] and (2) mom must pass the allele to child:
- Probability of mom being carrier = 1/100
- Probability of mom passing on disease allele = 1/2
Puting it all together. Now, combine all together:
= (probability of dad being carrier) * (probability of dad passing on disease allele) * (probability of mom being carrier) * (probability of mom passing on disease allele)
= 2/3 * 1/2 * 1/100 * 1/2
= 1 in 600
Here’s another very nice one that superimposes the pathway onto a simplified brainstem drawing (nice for the anatomical relations):
https://webeye.ophth.uiowa.edu/eyeforum/cases-i/case252/Fig2-INO-LRG.png
Source article:
https://webeye.ophth.uiowa.edu/eyeforum/cases/252-internuclear-ophthalmoplegia.htm
To see even more, try google image search on “medial longitudinal fasciculus”:
https://www.google.com/search?q=medial+longitudinal+fasciculus&tbm=isch
Nice schematic of how horizontal gaze is coordinated through the abducens/MLF/oculomotor pathway:
https://n.neurology.org/content/neurology/70/17/e57/F1.large.jpg
In the diagram, the system is coordinating gaze toward pt’s left, which (conveniently) is the same as in the stem.
Source article: https://n.neurology.org/content/70/17/e57
The stem is describing sequelae of posterior inferior cerebellar artery occlusion, resulting in Wallenberg syndrome. Here’s a nice schematic of the affected nuclei and brain stem regions:
https://i.ytimg.com/vi/A8S3B9p1t_g/maxresdefault.jpg
... and a 6-minute YouTube video that walks you through it:
https://www.youtube.com/watch?v=A8S3B9p1t_g
After the cuff is tied, the cells and tissue distal to the cuff will continue consuming ATP (ATP->ADP), but no fresh blood will be delivered to “clear” what will be an accumulating amount of ADP and other metabolites. ADP (=Adenosine) is itself a proxy of consumption and drives vasodilation of arteries! (Evolution is smart!) Increasing ADP/Adenosine in a “local environment” is a signal to the body that a lot of consumption is occurring there; thus, arteries and arterioles naturally dilate to increase blood flow rates and “sweep away” metabolic byproducts.
EBV is not a “respiratory virus” -- it’s a B cell virus. It infects B cells; not laryngeal cells.
Even though you might associate it with the “upper respiratory tract” (=kissing disease), it doesn’t cause respiratory inflammation since that’s not its trope. B cells are its trope! That’s why EBV is implicated in Burkitt Lymphoma, hairy leukoplakia and other blood cancers. (EBV is also known as “lymphocryptovirus” -- it was originally discovered “hiding” in lymphocytes of monkeys.) So, EBV = think B cells. From the MeSH library:
The type species of
LYMPHOCRYPTOVIRUS, subfamilyGAMMAHERPESVIRINAE, infecting B-cells in humans. It is thought to be the causative agent ofINFECTIOUS MONONUCLEOSISand is strongly associated with oral hairy leukoplakia (LEUKOPLAKIA, HAIRY;),BURKITT LYMPHOMA; and other malignancies.
https://meshb-prev.nlm.nih.gov/record/ui?name=HERPESVIRUS%204,%20HUMAN
[deleted]
Also consider this great description from the NIH’s MeSH database:
INCIDENCE: The number of new cases of a given disease during a given period in a specified population. It also is used for the rate at which new events occur in a defined population. It is differentiated fromPREVALENCE, which refers to all cases, new or old, in the population at a given time.
https://meshb.nlm.nih.gov/record/ui?ui=D015994
Don’t forget that incidence is the number of new cases which emerge in an unaffected population. Incidence is trying to get at the question -> “In a given year, how many new people develop this disease?”
In other words, you cannot count people who already have the disease. You have to exclude those people from your calculation. You want to know, among all the people out there who DO NOT have the disease, how many times this year was someone (newly) diagnosed?
Said differently still, you don’t want to “double-count” people who developed the disease before your study. As an epidemiologist, that would screw up your sense of how infective or transmissible a disease is. You want to know, “from time1 to time2 how many new cases emerged?”
2,500 students ... but you find out during your initial screen that 500 already have the disease. So, strikeout those people. That leaves 2,000 students who don’t have the disease.
Over the course of 1 year, you discover 200 students developed the infection. Thus:
200 new cases / 2,000 people who didn’t have the disease when you started your study = 10 percent
Tricky, tricky NBME ...
The synthesis of virtually all proteins (mRNA->peptide) occurs in the cytoplasm.[1] That’s where all ribosomes reside, after all. Ribosomes, which are mostly just rRNA (~2/3 rRNA + 1/3 protein*, by weight), are assembled in the nucleus but only do their stuff once they get to the cytoplasm.
For a protein to leave its original hometown of the cytosol and become a resident of the nucleus or, say, the endoplasmic reticulum, it needs to have a little string of amino acids which shout “I belong in the nucleus!” or “I belong in the endoplasmic reticulum!”
Proteins ultimately destined for the ER contain an unimaginatively named string of amino acids known as “signal sequence,” which, for the purposes of the Step 1, is always at the N-terminus. The signal sequence tells other cytosolic proteins, “Hey! Take me (and the rest of the peptide of which I am part) to the ER!”
In the absence of this signal, a protein will remain in its “default” home of the cytosol.
Here’s a nice schematic showing the flow of proteins from initial synthesis to final destinations:
Endnotes
- “The synthesis of virtually all proteins in the cell begins on ribosomes in the cytosol.” (Essential Cell Biology, Alberts et al., 2014, p. 492)
*If you really want your mind blown, consider that even the protein subunits that make up that 1/3 of a ribosome are themselves initially synthesized in the cytosol; later, they are transported back into the nucleus via the nuclear pore.
Here’s one way to process-of-eliminate “decreased hydrogen-bond formation”: I’m not a big fan of this line of reasoning, but technically alanine as a side group has more hydrogens* for potential hydrogen bonding than glycine:
alanine: —CH3
glycine: —H
So, “technically,” alanine would permit more hydrogen-bond formation, which might allow you to eliminate that choice.
That said, it seems almost impossible to rule out (without very technical knowledge or some provided experimental data) that the slightly larger alanine does not impair hydrogen bonding between collagen molecules via steric (spatial) interference. In simpler terms, since alanine is larger, you would think that it must somehow interfere with the hydrogen-bonding that occurs with the wild-type glycine.
---
*Strictly speaking, it’s not the number of hydrogens but also the strength of the dipole that facilitates hydrogen bonding: a hydrogen bound to a strongly electronegative molecule like fluorine will “appear” more positive and, thus, hydrogen-bond more strongly with a nearby oxygen (compared with a hydrogen connected to carbon, for example).
Further reading:
Vasoconstriction (narrowing of a tube) will cause the flow rate to increase through that tube, which decreases radial/outward pressure. The faster a fluid moves through a tube, the less “outward” force it exerts. (This is known as the Venturi effect.)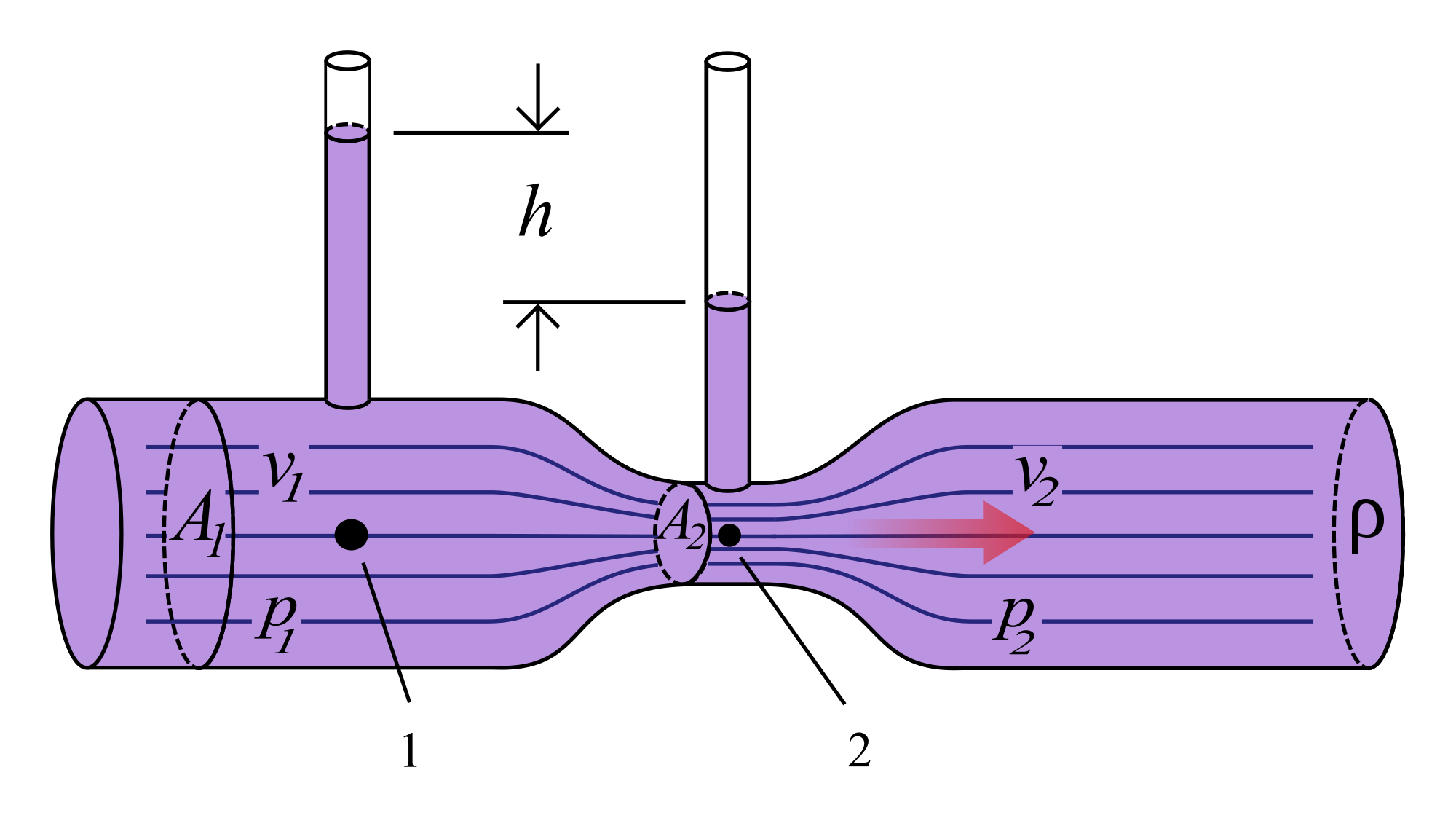
This is an interesting one. I like to remember it this way: in people with narcolepsy, all the “right kinds” of sleep are happening at all the “wrong times” of day. During the day, when a power nap would typically throw you immediately into REM, this kid is only entering Stage 1 or 2 (lightest sleep = slightest noises jar him back to reality). At night, when he should peacefully drift into Stage 1, 2, and so on, he instead completely zonks out. Classic narcolepsy.
From UpToDate: “Narcolepsy can be conceptualized as a disorder of sleep-wake control in which elements of sleep intrude into wakefulness and elements of wakefulness intrude into sleep.”
The more general principle: endothelia vasodilate in the presence of high CO2; you gotta get rid of that acid somehow! Can’t let it accumulate, as lower pH within a “micro-environment” affects structure/efficiency of enzymes, proteins, etc. The more acidic a local environment, the more you expect nearby vasculature to dilate (as a means of increasing flow rate, thereby ferrying off accumulate acid).
The anesthesiologist can exploit this mechanism. By hyperventilating (blowing off CO2), the brain vasculature senses a low CO2 / “hunky-dory state,” which requires no vasodilation. In other words, the vasculature does not need to continue the ATP-consuming practice of synthesizing Nitric Oxide (NO).
This is essentially a formal logic question. Logically speaking, the question asks us to identify a mechanism that tumor suppressors have which proto-oncogenes do not. In other words, what is a mechanism shared by all known tumor suppressors but not shared by any known proto-oncogenes? For that reason, it can’t be phosphorylation; sure, phosphorylation is a mechanism of tumor suppressors but it’s also a mechanism of many known proto-oncogenes.
Inability to maintain an erection = erectile dysfunction. So now the question is "Why?"
Fatigue, difficulty sleeping, difficulty concentrating is starting to sound like depression. "Difficulty concentrating" might be interpreted as impaired executive function or the beginnings of vascular-related dementia (dementia related to small but numerous cerebral infarcts), but on Step 1 dementia will be blatant (i.e., "lost his way home," "wandering," etc.).
Depression is actually common after a debilitating event like stroke, as you might expect. With depression comes a loss of sexual interest and desire—that is decreased libido.
One can make the argument that a "vascular patient" might have some issues with his "pipes" (arteriosclerosis, parasympathetic/sympathetic dysfunction) and, for this reason, nocturnal erection should be decreased; but note that nothing is mentioned about long-standing vascular disease (no hx of hypertension).
As a result, the best answer choice here is C. (Libido decreased but nocturnal erections normal.) The big question I have is, how the heck does this guy know he's hard when he's asleep!!? :p
The only reliable way to differentiate between PCP and cocaine on these exams: + nystagmus (not present here) + catatonia/sedation
Weird facts about PCP intoxication: + May wax and wane between extreme agitation and sedation + Blank stare and flat affect + Rigidity + May not have hypertension or tachycardia
I am NOT giving a stress test to every 50 year old male smoker with hypertension and family history of MI who wants to exercise. That would be so many patients and seems like a bad use of resources.
Tell me why I'm wrong. Is it because he has so many risk factors for CHD (age, sex, smoker, hypertension, family history)?
From UTD: "CHD screening tests are generally not recommended for asymptomatic patients, and cardiac stress testing should not be part of a routine annual physical or health screening examination. However, there are other patients in whom we perform stress testing: patients who need reassurance that it is safe for them to be active, in which a stress test can help providers delineate an activity program with specific levels of exercise to achieve; and patients who have an occupation in which high levels of exertion may be routinely required (eg, farmer)." https://www.uptodate.com/contents/screening-for-coronary-heart-disease
"Rare exceptions are patients with multiple risk factors" https://www.uptodate.com/contents/selecting-the-optimal-cardiac-stress-test
Can someone explain why cardiac output is high in septic shock?
Malignant pleural effusion. Cancer is full of protein.
Could someone explain to my why it is Factor X? Like I understand that PTT and PT are both elevated. I picked Factor X and then changed it to "hydrolysis of.." because I thought with a Factor X deficiency, wouldn't you have a prolonged thrombin time? I might be making this more complicated, but doesn't Factor X play a role in thrombin activation, so lack of it would lead to a prolonged thrombin time?
Why is it aphthous ulcers if there are no GI symptoms? Why can’t it be herpes zoster?
I get these VERY often. I seem to get them only after eating something that can damage the mucosa in my mouth such as hard chips (Tostitos, very jagged very pain). These are NOT cold sores (HSV). This is simply a aphthous ulcer; they can be stress induced (studying for hard test). they are very painful and do reoccur. there are no associated sx with them.
I get these VERY often. I seem to get them only after eating something that can damage the mucosa in my mouth such as hard chips (Tostitos, very jagged very pain). These are NOT cold sores (HSV). This is simply a aphthous ulcer; they can be stress induced (studying for hard test). they are very painful and do reoccur. there are no associated sx with them.
I thought of this as a giant physiologic shunt (ie, due to the pneumothorax there is no ventilation to an entire lung, as a consequence you retain CO2) - not sure if this is the actual mechanism but it helped me get this question right
hopefully this helps!
These are symptoms of acute benzo withdrawl
Can someone explain more on how to tackle these types of questions? I suck at these questions for real... To me, he sounded pretty sane and reasonable (does not wish to waste other people's money). Sure he might be under slight depression judging how he has a terminal illness and his statement on how nobody cares for him. But unless he is incoherent or displaying magical thinking, signs of loss of memory etc., why should he be evaluated on decision-making capacity?
Flow Rate = Velocity x Cross-Sectional Area
2 cm^2 x 20 cm/sec x 60 sec/min x 1 L/1,000 cm^3 = 2.4 L/min
1,000 cm^3 = 1 L
Flow Rate = Velocity x Cross-Sectional Area
2 cm^2 x 20 cm/sec x 60 sec/min x 1 L/1,000 cm^3 = 2.4 L/min
1,000 cm^3 = 1 L
Flow Rate = Velocity x Cross-Sectional Area
2 cm^2 x 20 cm/sec x 60 sec/min x 1 L/1,000 cm^3 = 2.4 L/min
1,000 cm^3 = 1 L
Flow Rate = Velocity x Cross-Sectional Area
2 cm^2 x 20 cm/sec x 60 sec/min x 1 L/1,000 cm^3 = 2.4 L/min
1,000 cm^3 = 1 L
Flow Rate = Velocity x Cross-Sectional Area
2 cm^2 x 20 cm/sec x 60 sec/min x 1 L/1,000 cm^3 = 2.4 L/min
1,000 cm^3 = 1 L
if you are 68 and still dating Palmala Handerson, your libido isnt low my friends.
If you knew that basement membrane disruption prevents restoration of normal tissue (repeat from another NBME), then you missed this because you didn't know what "preclude" means.
- High yield reference: https://www.merriam-webster.com/dictionary/preclude
- Does NOT mean "prior to"
Missing questions I miss due to lack of vocab and grammar, you love to see it
If you knew that basement membrane disruption prevents restoration of normal tissue (repeat from another NBME), then you missed this because you didn't know what "preclude" means.
- High yield reference: https://www.merriam-webster.com/dictionary/preclude
- Does NOT mean "prior to"
Missing questions I miss due to lack of vocab and grammar, you love to see it
Can someone please explain to me: If the posterior 1/3 of the tongue is developed from 3rd and 4th pharyngeal arches, why is it wrong to choose pharyngeal arch?
Just another piss poor government institution cutting corners. If you've done NBME 18 and seen the cell diagram figure it is the literal pinnacle
Graft Vs Host disease
Look out for
Skin involvement - maculopapular rash
Enteric involvement - diarrhea and or cramping , abdominal pain .. nausea/vomiting
Hepatic dysfunction - jaundice
*** The skin , liver and intestines are the most involved affected organs
FA 2020: 463
Causes of avascular necrosis: CASTS Bend LEGS. +Corticosteroids +Alcoholism +Sickle cell disease +Trauma +SLE
+“the Bends” (caisson/decompression disease) +LEgg-Calvé- Perthes disease (idiopathic) +Gaucher disease +Slipped capital femoral epiphysis
I think more generally, protein folding happens at the RER and the stem says the protein doesn’t fold properly. Specifically, the most common CF mutation is a misfolded protein and the protein is retained in the RER and not transported to the cell membrane - FA 2019 pg 60.
A medical student shouldn't be the one giving someone a cancer diagnosis. This is a really sensitive issue and the results should be given by someone with higher authority like a resident or attending. At the same time, you shouldn't lie to the patient and say that the results aren't back yet if they are. Best thing to do is deflect the conversation and follow up with the resident..
Tanner stages start at TEN years old
Stage I:
- I is flat, as in flat chest;
- I is alone, as in no sexual hairs.
Stage II (2): stage II starts at 11 y/o (II look like 11)
- 2 balls (testicular enlargement)
- 2 hairs (pubic hairs now appearing)
- 2 breast buds form
Stage III (3): starts at 13 y/o
- If you rotate 3, it looks like small breasts (Breast mounds form);
- If you squiggle the III they look like curly+coarse pubic hair
- Increased penis length and size can be represented by: II --> III
(your penis was thin II but now its thicker III)
Stage IV (4): starts at 14 y/o
- First imagine: The I in IV represents the thigh, and the V in IV looks like the mons pubis between your legs:
MEANING: you have hair in mons pubis (V) but you have a border detaining the hair from growing into thighs. - The V is pointy, as in now the breasts are pointy (raised areola or mound on mound)
Stage V (5): 15 y/o
- V has no borders detaining hair from growing into thighs (pubic hair + thigh hair)
- 5 fingers(as in hands) flattening the areolas when grabbing them (areola flatten at this stage and no more "mound on mound")
Male pattern baldness./androgenic alopecia is caused by the effects of dihydrotestosterone (DHT) on the skin of the scalp. Testosterone is converted by the enzyme 5-alpha-reductase into DHT. Finasterideis a 5-a-reductase inhibitor, and so blocks the production of DHT and can halt or even cause some reversal of make pattern baldness. However this same activity may also result in signficant sexual side effects including gynecomastia, erectile dysfunction, ejaculatory dysfunction, and decreased libido.
A) Danazol- a weak androgen with antiestrogenic effects, used in the treatment of endometriosis and fibrocystic breast disease. C) Methyltestosterone- synthetic T, it is used to supplement in testosterone deficiency, or in the treatment of some breast cancers. D) Oxandrolone- an anabolic steroid used to regain weight. E) Stanozolol- another anabolic steroid, with potential used for hereditary angioedema.
The important thing for most of the ethics questions are to look for the answer where you are being the nicest/most professional while respecting the patient’s autonomy, beneficence, non-maleficence, etc. Most of the choices here were either accusatory or basically being mean to the patient. The correct choice is to help the patient but also motivate them to continue physical therapy and to only use the permit as little as necessary. A similar question (which I think was on NBME 23 -- they are kind of blending together) was the one where the patient had test results that indicated he had cancer but the resident said not to (voluntarily) tell him until the oncologist came in later that day, and the patient asked you about the results. You don’t want to the lie to the patient and say you don’t know or that he doesn’t have cancer, but you also don’t want to be insubordinate to the resident’s (reasonable) request.
The important thing for most of the ethics questions are to look for the answer where you are being the nicest/most professional while respecting the patient’s autonomy, beneficence, non-maleficence, etc. Most of the choices here were either accusatory or basically being mean to the patient. The correct choice is to help the patient but also motivate them to continue physical therapy and to only use the permit as little as necessary. A similar question (which I think was on NBME 23 -- they are kind of blending together) was the one where the patient had test results that indicated he had cancer but the resident said not to (voluntarily) tell him until the oncologist came in later that day, and the patient asked you about the results. You don’t want to the lie to the patient and say you don’t know or that he doesn’t have cancer, but you also don’t want to be insubordinate to the resident’s (reasonable) request.
Mom and her daughter have the same sequence of FBN1. What is special is that compared to a “normal” (wild-type) FBN1, mom and daughter have one little tiny mutation in their sequence: a single nucleotide (A,T,G,C) that is different than most other folks.
(Interestingly, this nucleotide difference does not alter the amino acid encoded by this part of the gene; that makes Choice D (
change the folding of the protein) and Choice E (truncated protein) very unlikely.)Back to our question. Even though mom and daughter have the same mutation, mom shows no signs of Marfan syndrome; this eliminates Choice A (
disease-causing mutation in the patient and her mother).You might think this is an example of variable expressivity (not an option but a good guess), and it might be.
In the stem they say:
Interesting! This means that in a “normal” sample of people (who have no signs of Marfan), 15 out of 200 still have this mutation.
(They don't say anything about how many Marfan people have the mutation but we don't need that information to answer the question.)
When a gene can be found in multiple “versions”, we call the gene polymorphic (literally,
many-shapesormany-forms).So the best response is Choice B (
polymorphism).